The Centers for Medicare & Medicaid Services (CMS) has officially released the Contract Year (CY) 2027 Notice of Intent to Apply (NOIA) for Medicare Advantage (MA) and Part D plans. Health plans preparing for new or expanded contracts should act quickly: several critical submission deadlines fall between November 2025 and February 2026.
The NOIA process is the first required step for organizations planning to offer new Medicare Advantage or Prescription Drug Plan products, expand service areas, or modify existing contracts for CY 2027.
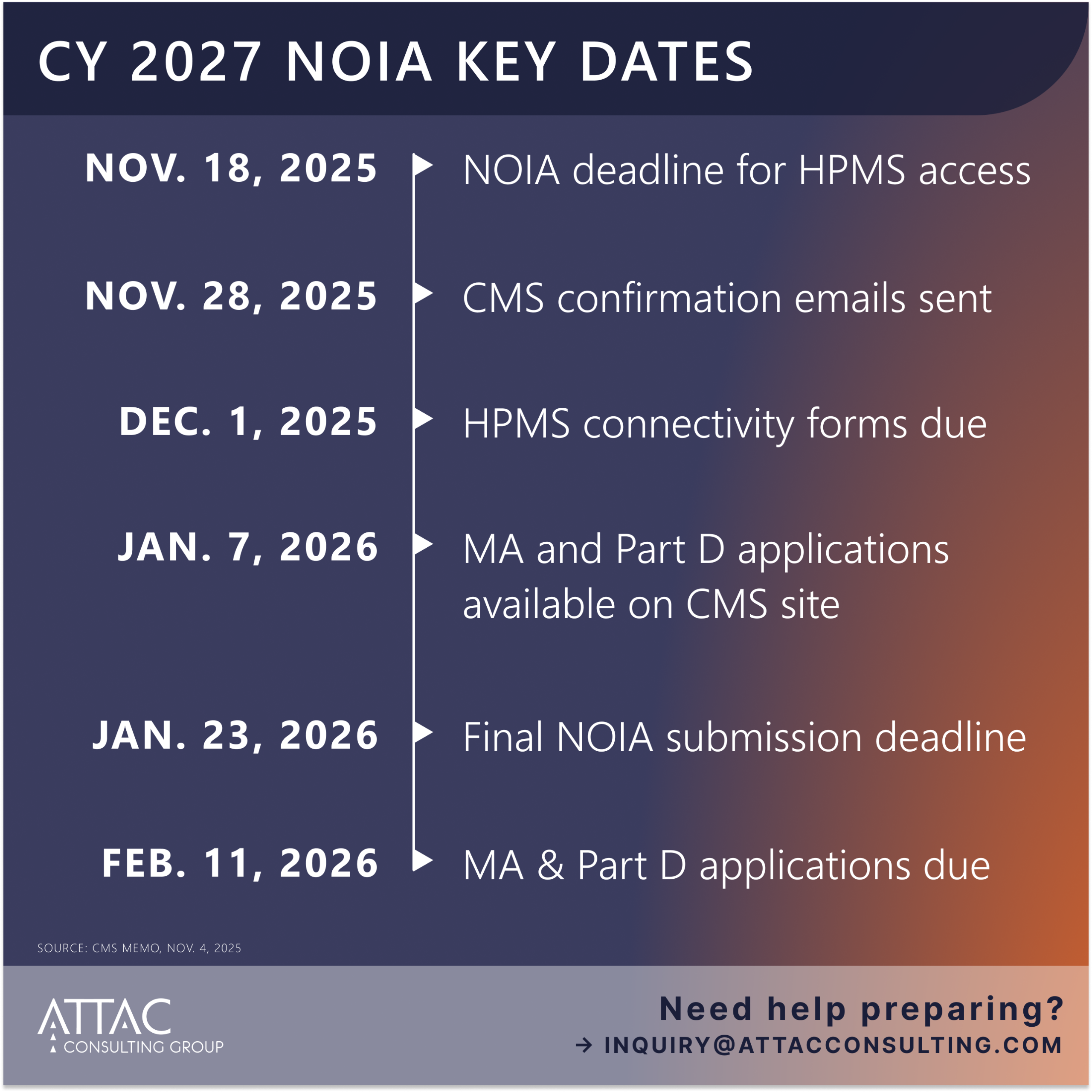
Key CY 2027 NOIA Deadlines
| Deadline | Action |
|---|---|
| November 18, 2025 | NOIA deadline to ensure access to CMS Health Plan Management System (HPMS) |
| November 28, 2025 | CMS sends confirmation emails for organizations meeting the Nov. 18 deadline |
| December 1, 2025 | HPMS User ID connectivity forms due |
| January 7, 2026 | MA and Part D applications available on CMS website |
| January 23, 2026 | Final NOIA submission deadline |
| February 11, 2026 | MA and Part D applications due to CMS |
Source: CMS Memo, November 4, 2025
What This Means for Health Plans
CMS reminds applicants that submitting a NOIA by November 18, 2025, ensures full access to HPMS once the MA and Part D applications are released in January. While CMS will continue to accept NOIAs
through January 23, 2026, plans submitting after November 18 risk reduced time to complete and submit their applications.
Organizations seeking new or expanded MA or Part D contracts should review the NOIA requirements closely. CMS has outlined specific rules for:
- New plan types such as HMOs, PPOs, MSAs, and PDPs
- Service area expansions (SAEs)
- Dual-Eligible Special Needs Plans (D-SNPs) and Institutional SNPs (I-SNPs)
- Network-based PFFS transitions
Plans offering new MA products or expanding into new regions must also prepare to demonstrate compliance with network adequacy standards under 42 CFR § 422.116, which requires timely submission of Health Service Delivery (HSD) tables.
Network Adequacy: Don’t Leave It to the Deadline
CMS encourages plans to prepare and submit network adequacy documentation early, emphasizing that last-minute HSD submissions can lead to technical errors or missed exceptions. For plans expanding or entering new markets, this process often represents one of the most complex and time-consuming parts of the MA application.
That’s where ATTAC’s Provider Network Management teams can help. Our experts assist plans with:
- Building compliant networks that meet CMS time-and-distance standards
- Validating provider data across multiple systems
- Conducting access and availability surveys to demonstrate adequacy
- Streamlining submissions and reducing administrative burden through proven processes and technology
Stay Ahead of the NOIA Timeline
The NOIA clock is already ticking: and early preparation can make the difference between a smooth approval and a last-minute scramble.


