Regional Health Plan Boosts Risk Accuracy and ROI Through Targeted Retrospective Chart Review
 A regional payer operating across multiple states wanted to close a long-standing gap in risk score accuracy across its Medicare Advantage and ACA lines of business. Despite conducting routine retrospective chart reviews and following best practices, results lagged behind peers. The plan worried that expanding review volume would only drive up costs without delivering meaningful impact.
A regional payer operating across multiple states wanted to close a long-standing gap in risk score accuracy across its Medicare Advantage and ACA lines of business. Despite conducting routine retrospective chart reviews and following best practices, results lagged behind peers. The plan worried that expanding review volume would only drive up costs without delivering meaningful impact.
The Challenge: A Persistent Gap in Risk Accuracy
Ongoing gap in risk score accuracy compared to competitors
Limited scope in existing retrospective reviews leading to undercoding
Concern about diminishing returns from expanding review volume
The ATTAC Approach: Data-Driven Targeting and Expansion
ATTAC’s team analyzed the plan’s historical results using advanced analytics to pinpoint missed opportunities in their targeting logic. Within a single week, we:
Redesigned and expanded chart-targeting parameters to capture a broader and deeper set of records
Modeled cost vs. return to maintain strong ROI
Deployed an enhanced retrospective review program focused on precision and audit-defensible accuracy
The Results: 4:1 ROI and $2M in Incremental Impact
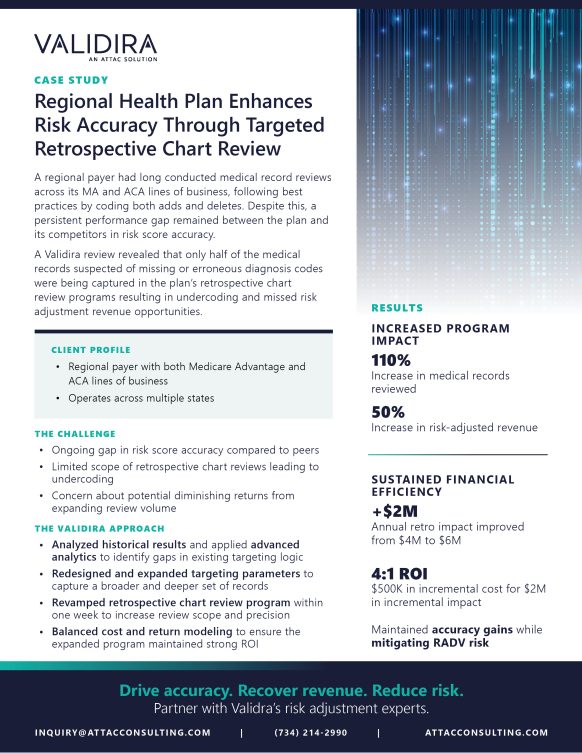
The enhanced targeting and expansion effort increased medical records reviewed by 110%, producing a 50% increase in risk-adjusted revenue without compromising coding integrity. The program achieved a 4:1 ROI, delivering $2 million in incremental impact with just $500K in added cost.
By improving accuracy while mitigating RADV exposure, the plan achieved measurable and sustainable gains in both compliance and financial performance.
Outcome Highlights
+$2M annual revenue improvement
50% higher risk-adjusted revenue
110% increase in records reviewed
Maintained accuracy and RADV defensibility
ATTAC helps health plans drive accuracy, recover revenue, and reduce risk, all while keeping audit readiness front and center.

