CMS recently released updated operational guidance for Contract Year (CY) 2027 Medicare Advantage (MA) applications. This guidance introduces pivotal shifts in how organizations manage network adequacy and exception requests, meaning the “old way” of managing deficiencies is no longer sufficient for those preparing for the February submission.
Read More →In the Contract Year 2027 Proposed Rule (CMS-4212-P), CMS introduced significant changes to how provider network changes are handled, which will directly impact health plan operations and enrollment stability. For health plan leaders, the headline is clear: the proposed changes remove historical guardrails around network stability, potentially
Read More →As we close out 2025, the first year of mandatory secret shopper surveys under the CMS Final Rule is behind us. With the 2026 cycle starting on January 1, now is the time to apply the hard-won lessons from the inaugural reporting year. Reviewing the 2025 Access
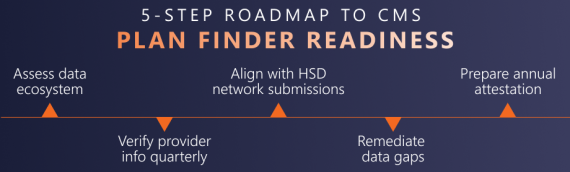
Read More →CMS Finalizes Medicare Plan Finder 2027 Rule: What Health Plans Need to Know In one of the most consequential transparency updates in recent years, CMS has finalized new requirements that will make Medicare Advantage (MA) provider directories publicly available on Medicare Plan Finder beginning with plan year 2027. This change marks a
Read More →The Centers for Medicare & Medicaid Services (CMS) has officially released the Contract Year (CY) 2027 Notice of Intent to Apply (NOIA) for Medicare Advantage (MA) and Part D plans. Health plans preparing for new or expanded contracts should act quickly: several critical submission deadlines fall between
Read More →In the 2025 Final Rule, CMS released its expectations and reporting requirements to ensure timely access to care. By the second Friday in June each year, issuers that offer Qualified Health Plans (QHPs)—including stand-alone dental plans—in the federally-facilitated exchanges or the federally-facilitated Small Business Health Options Programs
Read More →The new administration brings opportunities and challenges for the healthcare industry. While final regulatory guidance has not yet been released, health plans and providers will need to respond quickly when changes are finalized. An agile strategy, with the ability to rapidly deploy an expert workforce, is critical.
Read More →Are You Meeting CMS and State Access-to-Care Requirements? In the 2025 Final Rule, CMS released its expectations and reporting requirements to ensure timely access to care. Effective January 1, 2025, CMS requires issuers that offer Qualified Health Plans (QHPs), including stand-alone dental plans, to take specific actions.
Read More →Catch the webinar replay for expert insights on impacts of the CMS Final Rule. We discuss: Mental Health Parity | Significant changes will impact provider network operations and reimbursement. Provider Network Requirements | Tightened network adequacy standards are intended to ensure that plans provide beneficiaries with timely
Read More →By Jocelyn Bayliss The 2025 Final Rule from CMS outlined expectations and reporting requirements related to timely access to care. Effective PY 2025, CMS requires that all states with Medicaid and the Children’s Health Insurance Program (CHIP) develop, conduct, and enforce independent secret shopper surveys to evaluate
Read More →