CMS Finalizes Medicare Plan Finder 2027 Rule: What Health Plans Need to Know
In one of the most consequential transparency updates in recent years, CMS has finalized new requirements that will make Medicare Advantage (MA) provider directories publicly available on Medicare Plan Finder beginning with plan year 2027.
This change marks a fundamental shift: provider directory accuracy is no longer an internal compliance function: it’s about public accountability, member trust, and operational precision.
What’s Changing for Medicare Advantage Plans
Under the final rule, MA organizations must:
- Submit the provider directory directly to CMS for publication on Medicare Plan Finder beginning with 2027, prior to open enrollment.
- Update provider information within 30 days of becoming aware of any changes.
- Attest at least annually that directory information is accurate and complete.
To prepare for that transition, CMS will use third-party data sources to populate provider details for the 2026 Plan Finder update, effectively setting a benchmark for how complete and reliable each plan’s data appears before plans themselves assume responsibility in 2027.
While CMS did not finalize a proposal requiring direct attestation that directory data match network adequacy submissions, plans are still expected to maintain consistency between both datasets. The message is clear: network accuracy and directory accuracy must align.
Why This Matters: From Compliance to Public Accountability
For MA organizations, this is not a one-time compliance project. It’s an ongoing operational transformation that will require:
Quarterly (or more frequent) data verification cycles
Plans that have not yet implemented routine provider verification cycles must do so now to maintain compliance with the 30-day update requirement.
System interoperability and workflow redesign
Most plans still maintain fragmented data across multiple systems: claims, credentialing, directory, and contracting. Integrating these sources is essential to ensure that updates cascade accurately.
Governance and cross-departmental oversight
Attestation processes will need to include documented verification steps, clear accountability, and cross-departmental oversight between Provider Network, Compliance, and IT teams.
Strategic use of analytics
Plans should leverage data analytics to proactively flag inconsistencies, identify inactive or retired providers, and detect mismatched location data before CMS, and members, view them online.
In short, the 2027 rule turns directory accuracy into an enterprise-wide readiness issue, with implications for compliance, member experience, and brand reputation.
A 5-Step Readiness Roadmap
Plans should begin preparing now, well ahead of 2027 open enrollment. ATTAC recommends the following phased approach:
Assess your current provider data ecosystem
- Identify all systems contributing to your provider directory and map data flows between them.
- Identify all systems contributing to your provider directory and map data flows between them.
Implement continuous verification protocols
- Move from annual validation to quarterly reviews of provider practice locations, affiliations, and availability.
- Move from annual validation to quarterly reviews of provider practice locations, affiliations, and availability.
Align directory and HSD network adequacy data
- Ensure your directory data reflects the same provider details and specialties used in Health Service Delivery (HSD) network filings, particularly for plans undergoing service area expansions due in early 2026.
- Ensure your directory data reflects the same provider details and specialties used in Health Service Delivery (HSD) network filings, particularly for plans undergoing service area expansions due in early 2026.
Remediate gaps and update provider records
- Use findings from your accuracy checks to address both immediate gaps and systemic issues, including provider outreach, contracting updates, and technology integration.
- Use findings from your accuracy checks to address both immediate gaps and systemic issues, including provider outreach, contracting updates, and technology integration.
Build attestation documentation and governance
- Develop internal controls and documentation processes that can support annual certification of directory accuracy to CMS.
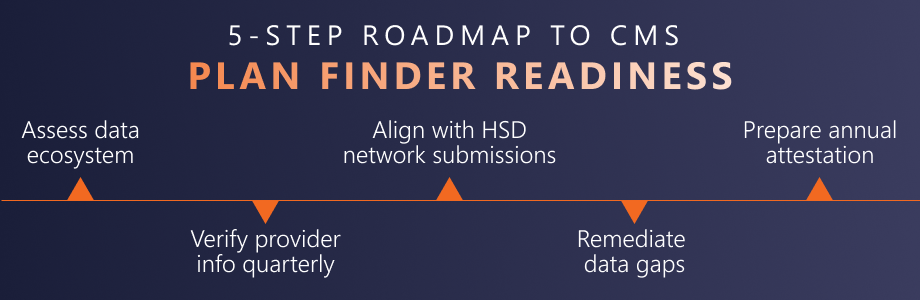
A 5-step roadmap outlining how Medicare Advantage plans can prepare for CMS Plan Finder requirements by 2027.
Beyond Directories: A Data Integrity Imperative
This rule is part of CMS’s broader effort to strengthen member access and transparency. For plans, the implications extend well beyond directory management. Accurate provider data underpins network adequacy, member access, quality reporting, and risk adjustment — all areas CMS monitors. Directory accuracy now affects every aspect of plan operations.
As provider directories become public-facing on Medicare Plan Finder, plans will be measured by the integrity of their data as much as by their benefits.
How ATTAC Helps Plans Stay Ready For CMS’s New Provider Directory Accuracy Requirements
ATTAC Consulting Group partners with Medicare Advantage, Medicaid, and commercial plans nationwide to build compliant, data-accurate provider network programs. Our experts combine regulatory insight, operational rigor, and analytics to help you move from reactive compliance to proactive accuracy.
Our teams work with plans to:
- Design continuous verification processes that meet CMS and Health Plan expectations,
- Build data reconciliation and governance frameworks, and
- Support network strategy and gap remediation aligned with HSD requirements.
Now is the time to prepare.
Medicare Advantage plans already collect and attest to the accuracy of their provider data but starting with the 2027 plan year, that data will become public through Medicare Plan Finder. This shift raises the stakes for accuracy, timeliness, and completeness.
Get ahead of 2027. Contact ATTAC to ensure your provider directory data is accurate, complete, and Plan Finder–ready.


