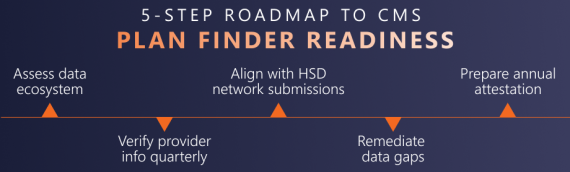
CMS Finalizes Medicare Plan Finder 2027 Rule: What Health Plans Need to Know In one of the most consequential transparency updates in recent years, CMS has finalized new requirements that will make Medicare Advantage (MA) provider directories publicly available on Medicare Plan Finder beginning with plan year 2027. This change marks a
Read More →The Centers for Medicare & Medicaid Services (CMS) has officially released the Contract Year (CY) 2027 Notice of Intent to Apply (NOIA) for Medicare Advantage (MA) and Part D plans. Health plans preparing for new or expanded contracts should act quickly: several critical submission deadlines fall between
Read More →Regional Health Plan Boosts Risk Accuracy and ROI Through Targeted Retrospective Chart Review A regional payer operating across multiple states wanted to close a long-standing gap in risk score accuracy across its Medicare Advantage and ACA lines of business. Despite conducting routine retrospective chart reviews and following
Read More →
The Risk Adjustment Data Validation (RADV) rule was finalized by CMS in January 2023 to tighten oversight of Medicare Advantage (MA) plans. A central change was the removal of the fee-for-service (FFS) adjuster, which historically helped normalize error rates seen in MA and with those seen inRead More →
Kaiser Family Foundation Research released in August 2025 showed that one in four Medicare beneficiaries lived on less than $24,600 in income in 2024, and half lived on less than $43,200 [1]. Many have little or no savings, with 7.7 million enrollees spending more than 10% of
Read More →Charles Baker, VP, Compliance Solutions Congress may be stuck in partisan stalemates, but risk adjustment reform is one area where the gears are still turning. The No UPCODE Act (S.1105), introduced this spring, has quickly become the focal point for Medicare Advantage payment debates. What’s in the Bill? Chart reviews
Read More →Charles Baker, VP, Compliance Solutions Over the past three years, CMS hasn’t shouted, but it has indeed spoken. Quietly, steadily, and now unmistakably, the agency has cranked up oversight of Medicare Advantage and Part D plans. And the 2024 audit cycle? It’s not just louder— it’s broader, sharper,
Read More →In the HEALTHCARE STARcast, host Subbu Ramalingam breaks down the complex world of healthcare to reveal the real strategies and mindsets driving excellence. In this episode, Subbu Ramalingam talks with Charles Baker, Vice President of Compliance Solutions at ATTAC Consulting Group. Charles has worn many hats in
Read More →Charles Baker, VP, Compliance Solutions Tammy Hall, Sr. Consultant, Compliance & Health Plan Operations CMS began a deeper dive into utilization management (UM) for Part C services with the implementation of new UM requirements released in the 2024 Final Rule. On May 30, 2025, CMS raised the red
Read More →CMS is launching the most extensive RADV audit expansion in Medicare Advantage history. Health plans need to move quickly—and smartly—to reduce risk and limit exposure. One of the most common (and costly) mistakes? Contracting with the same vendors used for retrospective coding. Coders trained for retro reviews may bring
Read More →