Health plans should now prepare to implement changes, including developing member retention and acquisition strategies
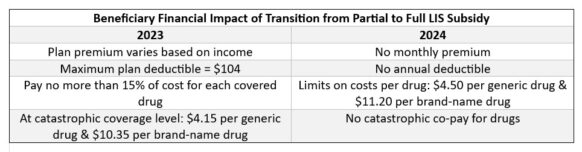
To improve access and affordability of prescription drugs for low-income beneficiaries, the Inflation Reduction Act of 2022 eliminated the partial low-income subsidy (LIS) benefit beginning in 2024. This change will move Medicare beneficiaries with incomes between 135% and 150% of the federal poverty level to the full LIS subsidy, also known as “Extra Help,” which helps pay for out-of-pocket Medicare prescription drug coverage. An estimated 300,000 beneficiaries who currently receive partial LIS will benefit from this change.
Additionally, in June CMS released new low-income subsidy data, estimating that approximately three million people are likely eligible for LIS but not enrolled. The release includes new key demographic information and a new outreach toolkit developed by CMS to help raise awareness about the program. The new data, along with efforts to increase awareness, is expected to increase LIS full subsidy enrollment.
Health plans should prepare now for implementation of the 2024 changes, including addressing impacts to:
- Benefits design and configuration
- PBM transactions and reporting
- Training and education for call centers, enrollment and billing, sales and marketing, providers, pharmacies, care management, and appeals and grievances
- Vendor/delegate/FDR contracts and operations
- Quality and risk adjustment outcomes
In addition to operational impacts, health plans will need to develop strategies to address potential gains and losses in membership.

Plans should now act to:
- Assess existing and potential membership
- Develop benefits, premium, retention, acquisition, marketing, communication, and education strategies
- Plan for implementation by:
- Developing effective, efficient project plans
- Assessing systems and operations
- Evaluating new model materials
- Developing proactive reporting and testing plans
- Preparing FDRs for implementation
- Educate staff, providers, pharmacies and FDRs
- Collaborate with community resources, providers and pharmacies to provide education and assistance to beneficiaries
Contact ATTAC Consulting Group about how our expert teams in technology, operations, provider network management, risk adjustment and compliance can provide your plan with comprehensive support with strategy, analysis, planning and implementation.

